Medical Ebook Review
OHI-S Regenerative Dentistry: PRF in Clinical Practice for Enhanced Healing and Recovery
In the continuously evolving field of dentistry, the integration of advanced techniques and materials is paving the way for enhanced patient care and treatment outcomes. One such remarkable innovation is the use of platelet-rich fibrin (PRF) in OHI-S regenerative dentistry. PRF has emerged as a game-changer due to its natural composition, biocompatibility, and regenerative potential. This guide delves into seven advanced applications of PRF within the realm of OHI-S regenerative dentistry, providing insights and practical knowledge essential for dental practitioners aiming to enhance their clinical practice.
Introduction to PRF in OHI-S Regenerative Dentistry
The landscape of dental practices is witnessing significant advancements, particularly in regenerative procedures that aim to restore oral health through biological means. Central to these innovations is the concept of OHI-S regenerative dentistry, which focuses on optimizing healing processes using the body’s natural resources. Among these resources, PRF stands out due to its unique properties that facilitate tissue regeneration and wound healing.
PRF is derived from the patient’s own blood and contains a rich concentration of growth factors, cytokines, and other biologically active components that promote healing. As dentists increasingly adopt the principles of regenerative dentistry, understanding and implementing PRF effectively can lead to improved treatment outcomes, reduced recovery times, and ultimately, increased patient satisfaction.
Understanding PRF in Regenerative Dentistry
To appreciate the significance of PRF in OHI-S regenerative dentistry, it’s essential to delve deeper into what PRF is and how it functions.
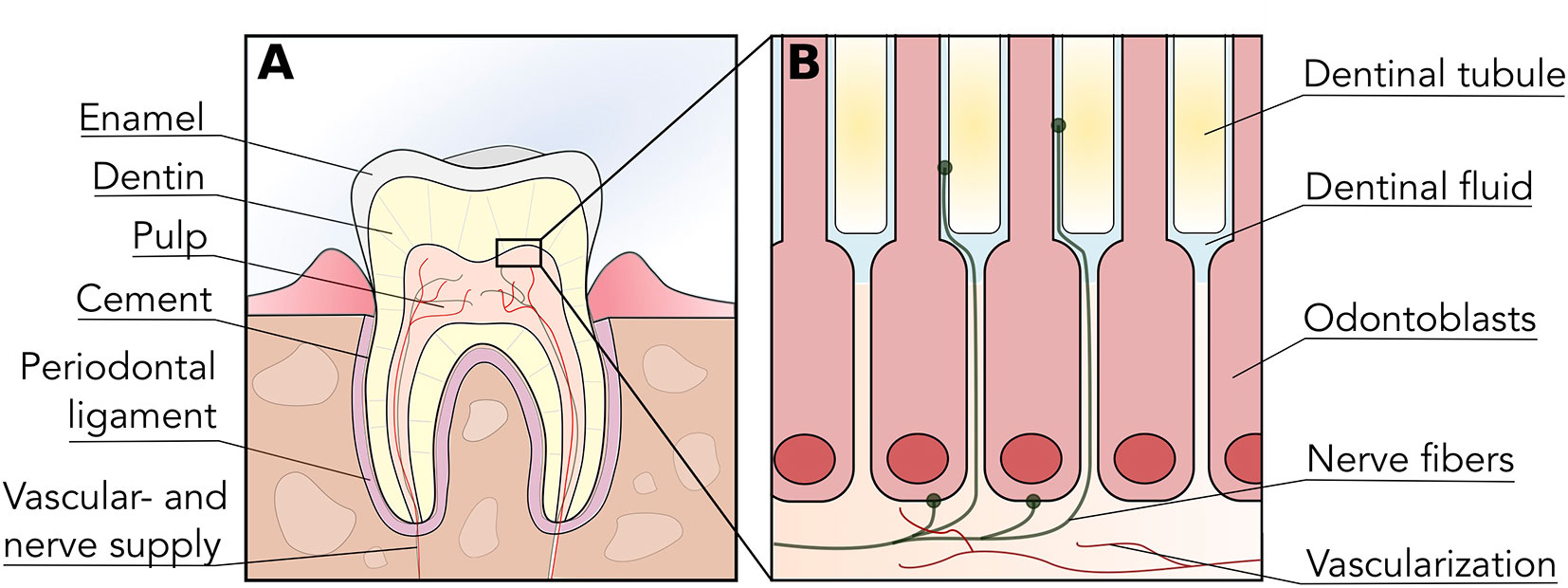
The science behind PRF and its regenerative properties
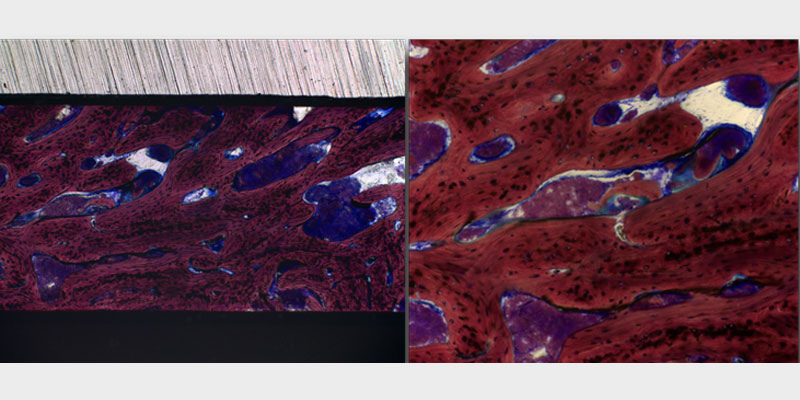
Platelet-rich fibrin is created by centrifuging whole blood, resulting in a fibrin matrix that entraps platelets and various growth factors. The scientific basis for PRF’s regenerative properties lies in its ability to release these growth factors over an extended period, promoting angiogenesis, osteogenesis, and soft tissue healing.
When applied in clinical practice, PRF stimulates stem cells in the surrounding tissues, enhancing their capacity to proliferate and differentiate into necessary cell types. This process is vital in procedures such as bone grafting, periodontal surgery, and implant placements where efficient healing is crucial.
Benefits of PRF in OHI-S dental procedures
Utilizing PRF in OHI-S procedures comes with numerous advantages. Firstly, being derived from the patient’s blood minimizes the risk of allergic reactions or disease transmission, making it a safe choice for most patients.
Moreover, the incorporation of PRF can enhance the overall success rates of various dental treatments. It not only accelerates the healing process but also helps in minimizing postoperative complications. For example, in periodontal therapy, PRF has been shown to promote better attachment levels and reduce pocket depth compared to traditional methods.
Further, by utilizing PRF, practitioners can create a minimally invasive treatment approach that enhances patient comfort and satisfaction. With faster healing times and less discomfort associated with post-operative recovery, both the practitioner and patient benefit significantly.
PRF Preparation Techniques for OHI-S Clinical Practice
Successful application of PRF in clinical settings requires proper preparation techniques. Understanding these methods ensures optimal outcomes in all regenerative dental procedures.
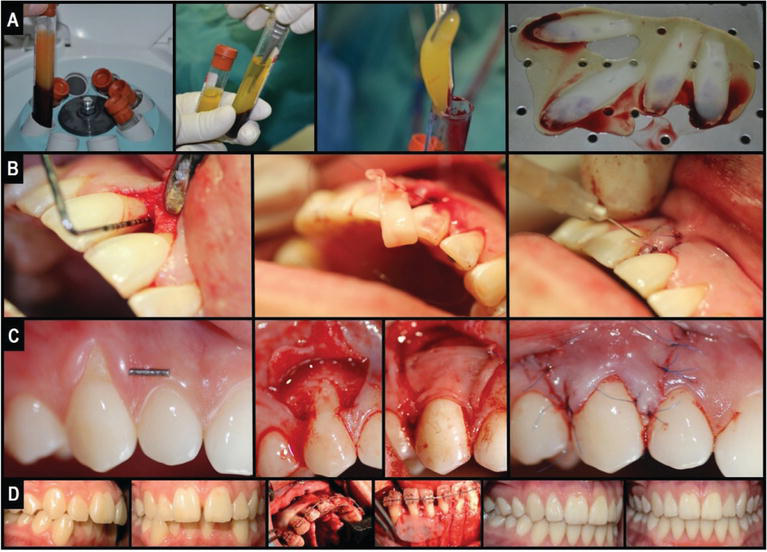
Step-by-step guide to preparing PRF in a dental setting
The preparation of PRF involves several critical steps that must be followed meticulously to ensure the highest quality product. The process begins with drawing blood from the patient, usually collected in specific anticoagulant-free tubes.
Once the blood is drawn, it is placed in a centrifuge which separates the components according to their density. Typically, a two-step centrifugation technique is employed, first at a low speed to segregate red blood cells, and then at a higher speed to concentrate the platelets and fibrin at the top layer.
After centrifugation, the PRF is carefully harvested using sterile instruments to avoid contamination. This prepared PRF can then be utilized directly in various applications, either as a gel or membrane, depending on the clinical requirement.
Equipment and materials needed for PRF preparation
To prepare PRF efficiently, certain key equipment and materials are essential. A reliable centrifuge that allows for variable speeds and precise control over the duration is crucial. Most dental practices will need specialized PRF tubes designed to optimize the separation process.
Additionally, standard surgical tools such as scalpel blades, forceps, and sutures will be required for harvesting and applying the PRF during procedures. Sterile conditions must always be maintained throughout the preparation process to prevent contamination, ensuring the efficacy of the PRF.
PRF in Periodontal Regeneration: OHI-S Approach
One of the most promising applications of PRF in OHI-S regenerative dentistry is its role in periodontal regeneration. The management of periodontal diseases often necessitates innovative solutions to restore lost tissue and improve functional outcomes.
Using PRF for guided tissue regeneration in periodontal defects
Guided tissue regeneration (GTR) is a well-established technique aimed at encouraging the growth of new periodontal tissue in sites affected by periodontal disease. The incorporation of PRF into GTR protocols enhances the regenerative capabilities by providing a rich source of growth factors that support the healing process.
When applied to periodontal defects, PRF acts as a scaffold, allowing for the sustained release of vital growth factors that facilitate cell migration and proliferation. This results in improved healing of the periodontal ligament, cementum, and alveolar bone, leading to better clinical outcomes in terms of probing depth reduction and attachment gain.
Case studies: Successful periodontal regeneration with PRF
Numerous case studies have illustrated the effectiveness of PRF in regenerating periodontal tissues. In one notable study, patients suffering from advanced periodontal disease underwent GTR combined with PRF application. The results demonstrated significant improvements in clinical parameters, including reduced pocket depths and enhanced clinical attachment levels.
These successful outcomes are attributed to the synergistic effects of PRF, which not only aids in tissue regeneration but also serves to modulate the local inflammatory response, creating a conducive environment for healing. By analyzing such cases, dental practitioners can gain confidence in adopting PRF in their periodontal treatment protocols.
Enhancing Bone Grafting Procedures with PRF in OHI-S Practice
Bone grafting is a common procedure in restorative dentistry, and PRF has been shown to enhance the success of these interventions.
Combining PRF with bone grafts for improved outcomes
For optimal bone regeneration, combining PRF with bone graft materials can yield superior results. Studies indicate that incorporating PRF into bone grafts enhances the material’s osteoconductive properties while accelerating the healing process.
PRF not only provides a favorable microenvironment for bone formation but also releases growth factors like transforming growth factor-beta (TGF-β) and vascular endothelial growth factor (VEGF), which stimulate angiogenesis and subsequent bone regeneration.
By utilizing this combination, practitioners can expect quicker osseointegration and enhanced stability of implants placed in grafted sites, ultimately leading to more predictable treatment outcomes.
PRF membranes: Applications in guided bone regeneration
Another innovative application of PRF in bone grafting is the creation of PRF membranes. These membranes serve as a barrier for guided bone regeneration (GBR) procedures, preventing the invasion of soft tissues while allowing for the desired bone growth.
The use of PRF membranes has several benefits, including biocompatibility and biodegradability, which contribute to a more natural healing process. Additionally, these membranes can be easily manipulated and shaped to fit the surgical site, further enhancing their applicability in various clinical scenarios.
As GBR techniques continue to evolve, the integration of PRF membranes represents a significant advancement in achieving successful bone regeneration.
PRF in Implant Dentistry: OHI-S Regenerative Approach
Implantology has greatly benefited from the use of PRF, which can address some of the challenges associated with implant placement and integration.
Using PRF for implant site preservation and development
In situations where there is insufficient bone volume for implant placement, PRF can play a pivotal role in site preservation and augmentation. By applying PRF to extraction sites immediately after tooth removal, clinicians can enhance the healing process and maintain the integrity of the alveolar ridge.
This proactive approach can minimize the occurrence of bone resorption, creating a more favorable environment for future implant placement. Additionally, the presence of growth factors in PRF aids in attracting osteogenic cells, further promoting the formation of new bone.
PRF-assisted implant placement and osseointegration
During and after implant placement, PRF can be utilized to enhance osseointegration—the process by which the implant fuses with the surrounding bone. By surrounding the implant with a PRF graft, clinicians can provide a richer source of growth factors that expedite the integration process.
Research has consistently shown that implants placed in conjunction with PRF experience faster healing and greater stability than those placed without it. As a result, incorporating PRF into implant procedures can significantly enhance the overall success rates of dental implants, benefitting both the dentist and the patient.
Soft Tissue Management with PRF in OHI-S Regenerative Dentistry
While bone regeneration is critical in many dental procedures, the management of soft tissues also plays a vital role in overall treatment success.
PRF for gingival recession treatment and soft tissue augmentation
Gingival recession is a common condition that can lead to aesthetic concerns and increased root sensitivity. The application of PRF for soft tissue augmentation presents a minimally invasive solution to this problem. By utilizing PRF in conjunction with connective tissue grafts or alone as a grafting material, clinicians can promote enhanced soft tissue healing and coverage over exposed roots.
The regenerative properties of PRF allow for improved vascularization of the graft site, leading to better integration and stability of the augmented tissue. Patients who undergo this treatment typically report higher satisfaction levels due to the cosmetic enhancements achieved.
Accelerating wound healing with PRF in oral surgery
In oral surgery, complications such as prolonged healing times or infections can adversely affect outcomes. The application of PRF in surgical sites serves to accelerate wound healing and reduce postoperative discomfort.
The growth factors found in PRF help to promote the formation of new blood vessels and connective tissue, thereby speeding up the healing process. Additionally, its anti-inflammatory properties can help mitigate swelling and discomfort following surgery, offering patients a more pleasant recovery experience.
Advanced PRF Techniques in OHI-S Sinus Lift Procedures
Sinus lift procedures can be challenging, yet PRF offers exciting opportunities to enhance success rates.
PRF-assisted sinus lift: Technique and benefits
A sinus lift procedure aims to increase the height of the maxillary sinus floor to accommodate implants. Integrating PRF into this procedure can yield substantial benefits, including improved bone regeneration and faster healing times.
Typically, PRF is placed within the augmentative material used during the sinus lift, providing a biologically active layer that promotes new bone formation. The growth factors released from PRF encourage local progenitor cells to migrate to the site, facilitating rapid and effective healing.
Managing complications in PRF-enhanced sinus augmentation
Despite the advantages of using PRF in sinus lifts, complications can still arise. Understanding how to manage these issues is crucial for maximizing the effectiveness of PRF in such complex procedures.
Practitioners should remain vigilant for signs of infection or inadequate bone formation. Early intervention, such as adjusting postoperative care or supplementing with additional growth factors or graft materials, can help mitigate these risks.
Equipping oneself with knowledge about current best practices and remaining adaptive can significantly influence the success of PRF-enhanced sinus augmentation.
Integrating PRF into Your OHI-S Regenerative Dental Practice
Adopting PRF into everyday practice requires strategic planning and training to maximize its benefits.
Developing a PRF protocol for your clinic
Establishing a standardized protocol for PRF preparation and application is essential for ensuring consistency and efficacy across all procedures. This protocol should encompass aspects such as patient screening, preparation techniques, storage, and application methods tailored to specific clinical scenarios.
Moreover, continuous assessment and refinement of the protocol based on clinical feedback and emerging research will help keep the practice at the forefront of regenerative dentistry.
Training staff and educating patients about PRF benefits
Education is crucial when integrating PRF into a dental practice. All team members must understand the science behind PRF, its preparation techniques, and its clinical applications. Regular training sessions, workshops, or seminars can foster an environment of learning, ensuring that everyone is equipped with the necessary skills.
Patient education is equally important. Clearly communicating the benefits and expectations associated with PRF procedures can help alleviate apprehension and build trust, ultimately leading to higher acceptance rates and satisfaction.
Common Pitfalls to Avoid When Using PRF in OHI-S Regenerative Dentistry
While PRF offers numerous benefits, pitfalls exist that practitioners must navigate to ensure successful outcomes.
Improper PRF preparation techniques
The efficacy of PRF is heavily dependent on the technique employed during its preparation. Inadequate centrifugation speeds, improper tube selection, or failure to maintain sterile conditions can compromise the quality of the PRF obtained.
Practitioners must adhere strictly to established guidelines and continually refine their techniques through practice and ongoing education.
Overestimating PRF capabilities in certain clinical scenarios
It is crucial for practitioners to recognize the limitations of PRF. While it has proven beneficial in many applications, it may not be suitable for every patient or situation. Overestimating its efficacy could lead to unrealistic patient expectations or suboptimal treatment outcomes.
Conducting thorough assessments and remaining honest with patients regarding the potential and limitations of PRF will help maintain professionalism and ethical standards within practice.
Frequently Asked Questions
How long does it take to see results from PRF in regenerative dental procedures?
The timeline for observing results from PRF varies depending on the specific procedure and patient response. Generally, initial healing can be seen within a few days, with more significant outcomes becoming evident within weeks to months as tissue regeneration progresses.
Is PRF safe for all patients in OHI-S regenerative dentistry?
While PRF is generally considered safe due to its autologous nature, certain medical conditions may contraindicate its use. Patients with blood disorders, certain autoimmune diseases, or those taking medications affecting coagulation should be thoroughly evaluated before PRF application.
Can PRF be combined with other regenerative materials in OHI-S procedures?
Yes, PRF can be effectively combined with other regenerative materials such as bone grafts or membranes. This combination can enhance the regenerative potential and improve clinical outcomes, provided that the materials used are compatible.
What are the contraindications for using PRF in dental treatments?
Contraindications for PRF use include patients with uncontrolled systemic diseases, significant blood disorders, or those undergoing anticoagulation therapy. A comprehensive medical history review is crucial to identify any potential risks.
How does PRF compare to other platelet concentrates in regenerative dentistry?
PRF distinguishes itself from other platelet concentrates primarily due to its three-dimensional fibrin matrix. This unique structure enables sustained release of growth factors over time, enhancing tissue healing and regeneration compared to other forms like platelet-rich plasma (PRP).
Conclusion
The advent of OHI-S regenerative dentistry marked a transformative shift in dental practices, emphasizing the importance of biological healing mechanisms. Within this framework, the use of PRF emerges as a potent tool, offering numerous applications that enhance treatment outcomes across various domains of dentistry.
By understanding the science behind PRF, mastering its preparation techniques, and integrating it thoughtfully into clinical practice, dental professionals can elevate their service offerings, ultimately benefiting their patients in profound ways. The future of regenerative dentistry is bright, and with continued exploration and innovation in PRF applications, the potential for improved patient outcomes seems limitless.